[COVID-19] Japan's Cluster-based Approach (Excerpt)
May 29, 2020
(Excerpt from the addendum of "Analysis of the Response to the Novel Coronavirus Disease (COVID-19) and Recommendations" of Expert Meeting on Novel Coronavirus Disease Control (May 29, 2020))
Counter-cluster measures concern conducting an active epidemiological investigation to ascertain the origin (source of infection, etc.) of the cluster of infections (outbreaks) and to take measures promptly so that the further spread of infections can be minimized and delayed. In Japan, it is believed that effective counter-cluster measures led to the following results.
(i) Large-scale spread of infection caused by a chain of clusters of patients was prevented.
(ii) Common sources of infection (the environment of 3C--closed spaces, crowded places, and close-contact settings) were identified through early, proactive epidemiological investigation. By raising awareness of these sources alongside additional factors such as singing and talking loudly, we were able to effectively deliver a message to citizens about avoiding as much as possible environments where clusters of infected patients (outbreaks) can occur.
(iii) By tracing the links of each infected person with a focus on clusters, the epidemic situation in each region was estimated more accurately. In other words, an increase in the number of "sporadic cases" whose links could not be traced was considered to indicate the spread of infection in a certain region, and this approach led to the early strengthening of regional measures.
That said, two characteristics should be noted.
(1) The spread of infection from China (the first wave) and the spread of infection from Europe, etc (the second wave) were detected early.
□ In the first epidemic wave from January to February which originated in China, 149 cases of infections were reported in Japan by February 25, including clusters of infected patients (outbreaks) as a result of the counter-cluster measures implemented by public health centers.
□ One factor behind such early reporting was that in preparation to host the Olympic and Paralympic Games, the concerned authority revised the criteria for suspected disease surveillance for early detection of unknown infectious diseases and called for early and broad reporting of suspected cases.
□ Meanwhile, in developed countries such as European countries and the US (excluding Italy where a serious local epidemic had already begun), as shown in the table above, few domestic infection cases had been detected at that point of time.
□ In reality, however, considerable spread of infection may have been already occurring beneath the surface in these countries, but the infections were not detected. By the time the infections were noticed, a rapid spread of infections had been exploded in Europe and the US after mid-March onward.
□ A reason behind Japan's early detection of infection was that medical care is easily accessible in Japan even in rural areas, and when an infectious disease such as COVID-19 was suspected due to a fever, respiratory symptoms, etc., doctors performed chest x-rays, CT tests, as well as PCR tests, resulting in the early detection of infection.
In fact, the first domestic case, which was confirmed on January 16, was found by a doctor who suspected infection and conducted a PCR test at his descretion.
(2) Effective counter-cluster measures were taken.
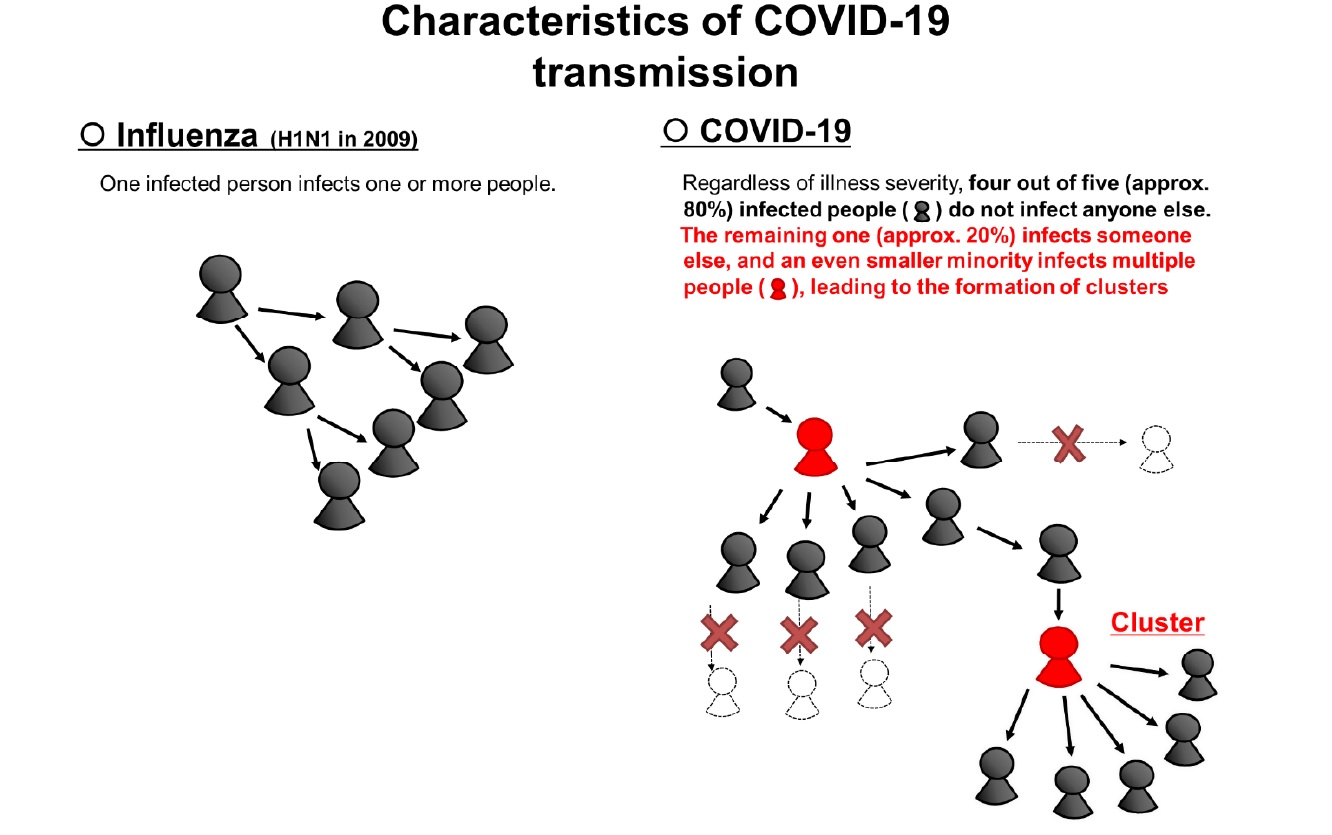
□ As described in (1), Japan succeeded in detecting new infections and clusters of patients earlier than other countries. By gathering these cases, the Expert Meeting recognized from early on 2 that this infectious disease has the characteristic that approximately 80 percent of the people who are confirmed to be infected, regardless of illness severity, do not infect anyone else, and that the characteristics clearly differ from those of the influenza virus, which is transmitted to others by many of those infected.
□ In other words, we had the perspective that this infectious disease spreads mainly by forming clusters, and that by suppressing the clusters, the spread of infection could be considerably reduced (as far as counter-cluster measures are taken).
□ Additionally, analyses of early active epidemiological investigations enabled us to analyze the settings in which clusters are likely to occur, leading to the discovery of the effective measures of avoiding the "3Cs," which other countries did not recognize.
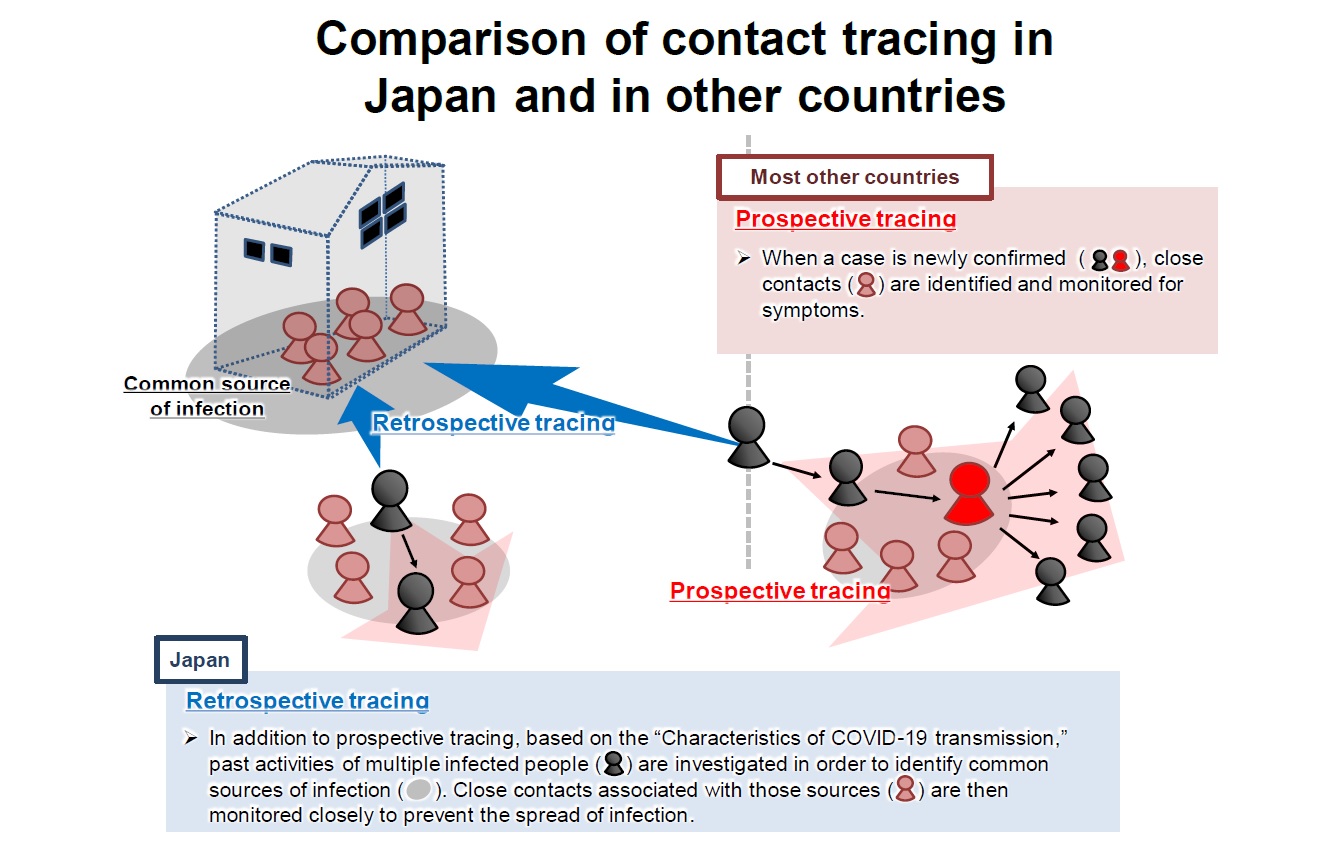
□ Contact tracing in other countries is "prospective" tracing, which begins with newly confirmed cases, identifies close contacts, and searches for future infection cases.
□ Japan performed such tracing too, but in Japan, based on the characteristics of this infectious disease, especially when multiple infected people have been observed, we additionally focus on identifying common sources of infection. In other words, when infected people were discovered, common sources of infection were identified retrospectively, which led to the early discovery of the concept of the "3Cs" that were common to such sources of infection. Additionally, from early on, emphasis was placed on conducting proactive epidemiologic al investigations thoroughly for those at the common source. Such retrospecti ve tracing was based in part on investigation methods traditionally used by public health centers for tuberculosis patients, etc.
□ In other words, Japan's measures are characterized by the aim to go back to the source of infection based on retrospective tracing so that the subsequent chains of infection are not missed. As a result, Japan focused on (i) identifying the source of infection early, (ii) identifying those associated with the source of infection early, and consequently (iii) providing medical care early, which (iv) led to making early efforts against the spread of infection.
□ As mentioned above, in Japan, by tracing the links of each infected person with a focus on clusters, the epidemic situation in each region was estimated more accurately. In other words, an increase in the number of "sporadic cases" whose links could not be traced was considered to indicate the spread of infection in a certain region, and this approach led to the early strengthening of regional measures.
□ Meanwhile, based on genetic analysis, the cases that entered from abroad are known to have largely influenced the spread of infection in Japan. Thus, as a result of cases entering from abroad at a larger scale, many sporadic cases occurred in different regions as the second wave from Europe, etc. In the surge of the number of new infections, such sporadic cases whose links could not be traced were also increased rapidly, which made a response based on the declaration of a state of emergency became unavoidable on April 7.
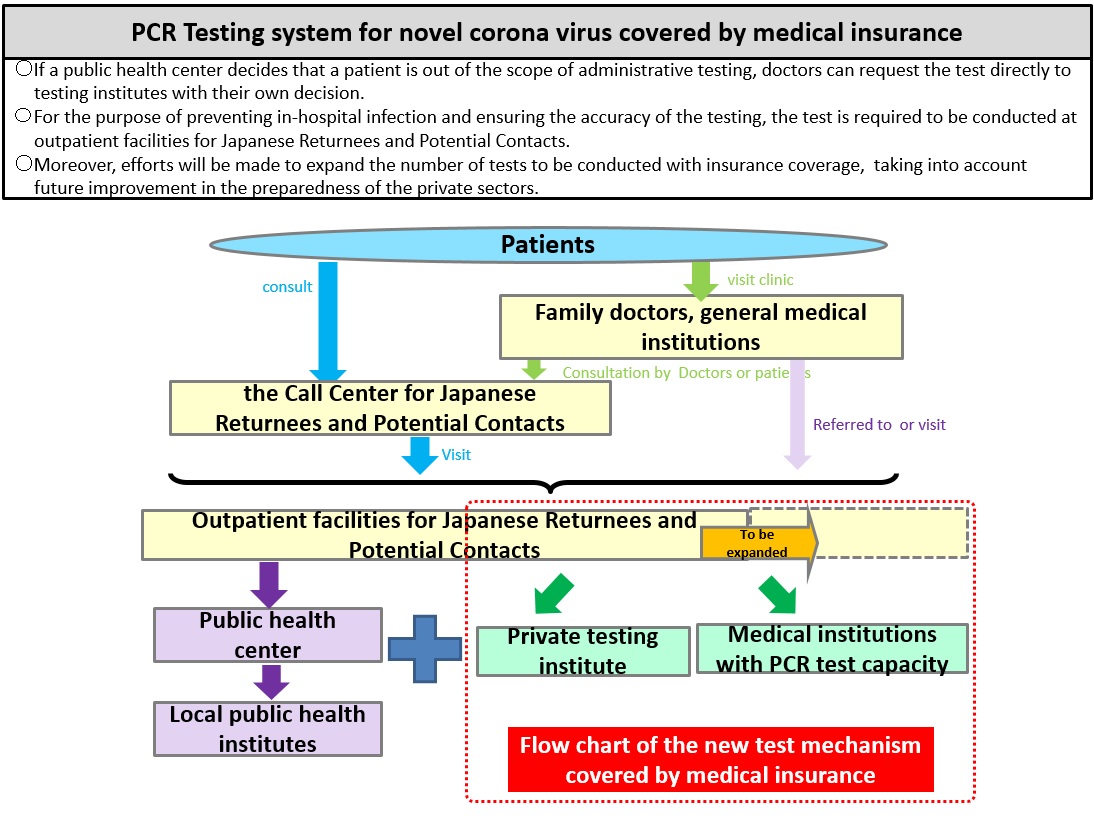
The rationale and structure of conducting PCR screening in Japan
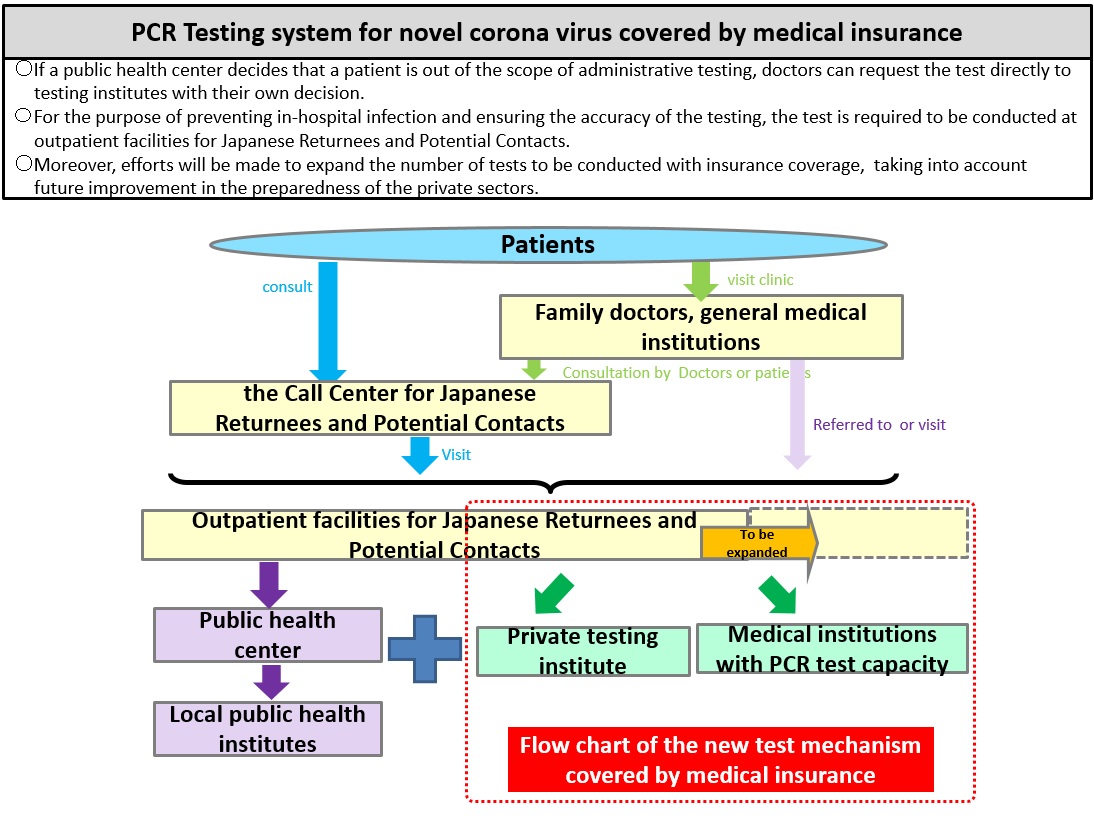
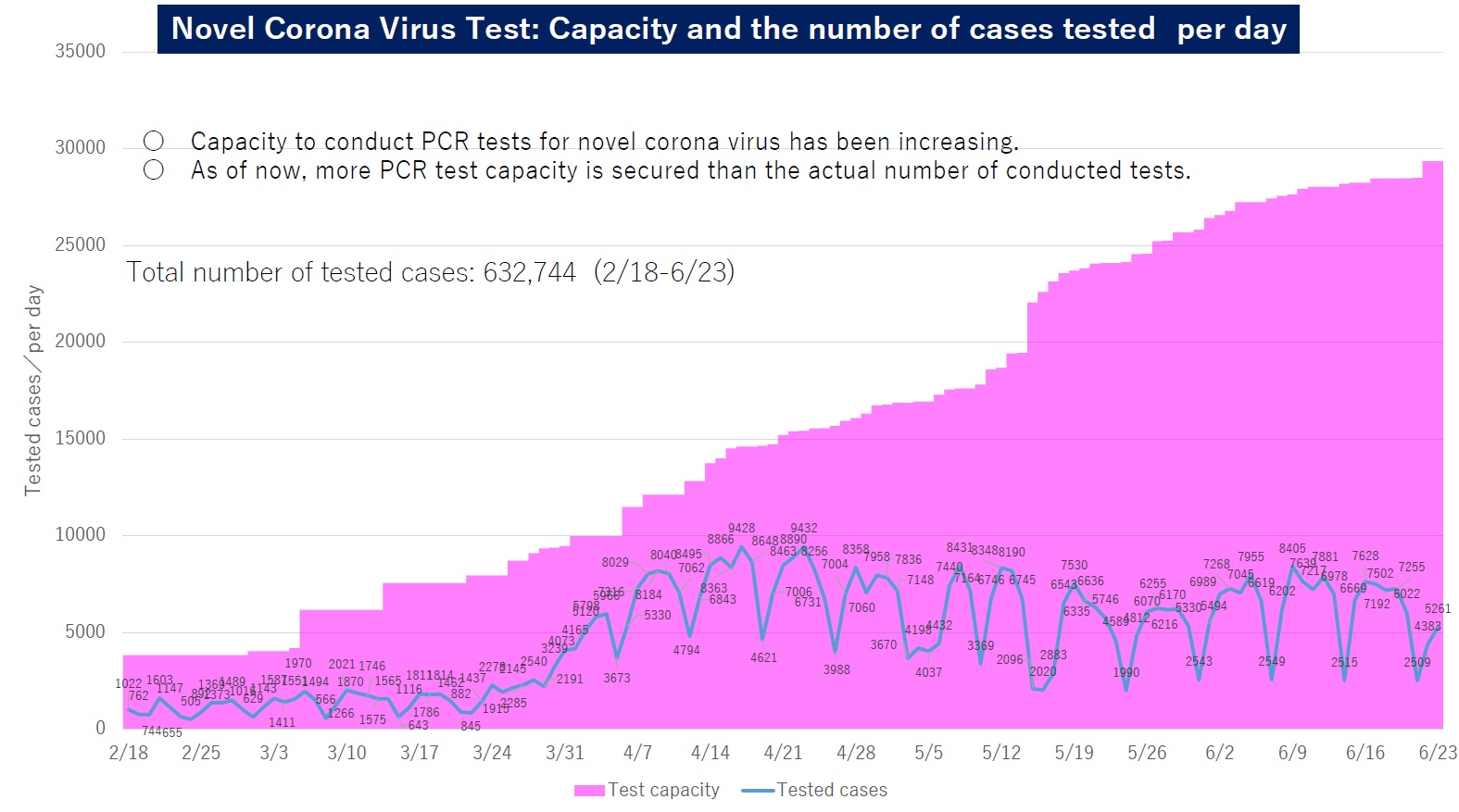
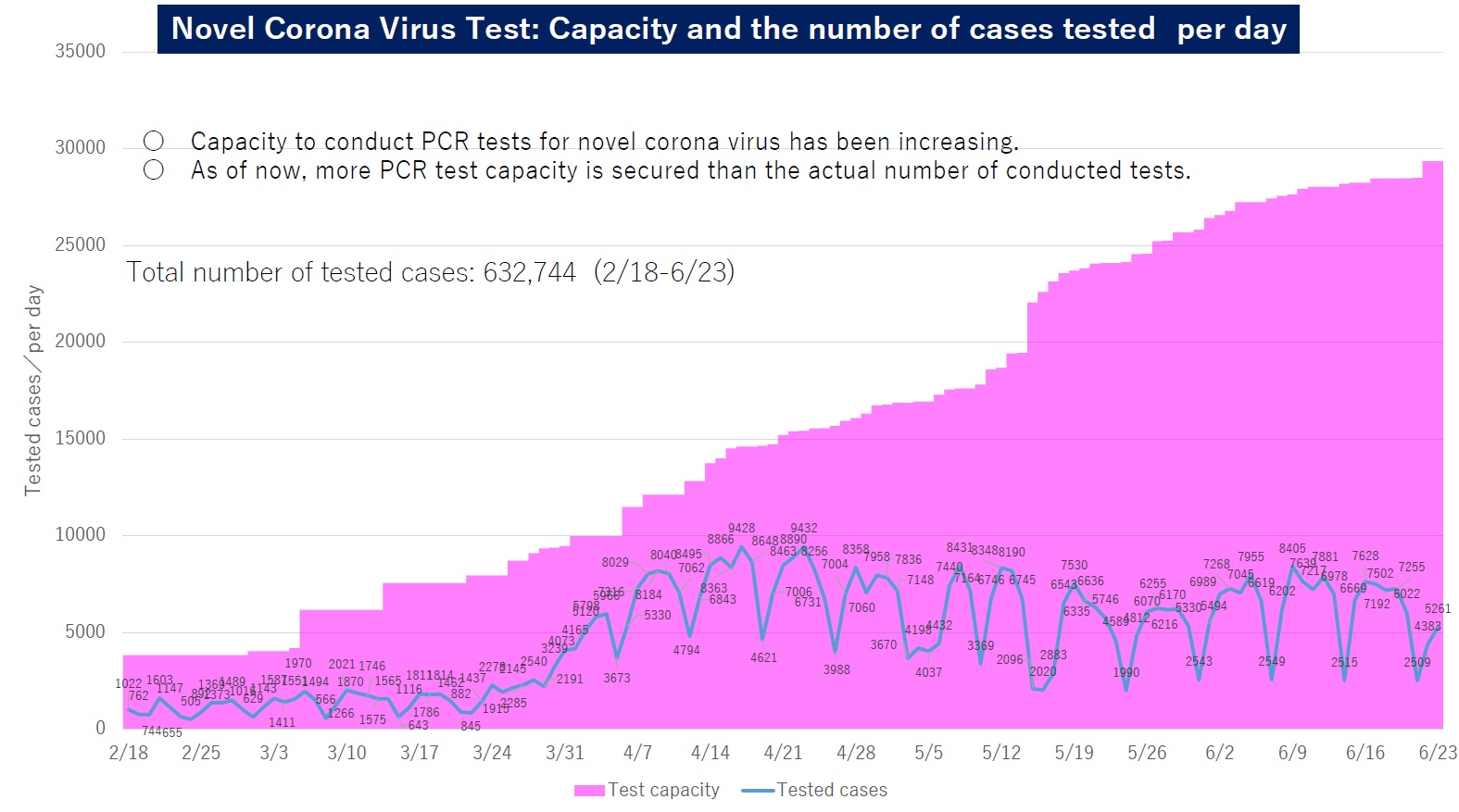
The government will ensure the sufficient PCR screening capacity so that all patients can receive PCR tests when doctors deem necessary.
PCR screening is now covered by health care insurance so as to facilitate the necessary tests for patients. Those who consult the Call Centers for Japanese Returnees and Potential Contacts (available 24 hours) and for whom it is deemed necessary to conduct screening by the respective outpatient facility for returnees and potential contacts, relayed by the call center, are eligible to request a test directly from one of the private-sector screening institutions without going through a public health center.
When medical doctors find necessary to conduct a PCR test, patients will be referred to outpatient facilities for returnees and potential contacts, and undergo screening based on the determination made by the doctors.
Aiming to prevent the refusal of test requests due to limited local screening capacity, the government will more closely facilitate the process to ensure that each area can conduct the necessary tests by sharing diagnostic reagents among wider areas.
At the same time, new rapid diagnostic test kits have been under development that can significantly shorten testing time.
(Reasons for requesting possible patients refraining from immediately consulting medical institutions)
First and foremost, most of the symptoms of a common cold, fever, lassitude, or difficulty in breathing, at this moment, are being caused by diseases other than the novel coronavirus disease, such as influenza. If a cold or influenza is suspected, it is advised to consult with a family doctor or other doctors nearby as usual.
Meanwhile, suspected patients of novel coronavirus are visiting outpatient facilities for returnees and potential contacts referred by the Call Centers for Japanese Returnees and Potential Contacts; when a person is not actually infected, visiting those medical institutions, which have outpatient facilities, without proper consultation, just because he or she is concerned about having an infection, will increase the risk of infection.
In the event of concern over infection by the novel coronavirus, it is advised to consult with the Call Centers. The list of medical institutions that have the aforementioned outpatient facilities is not disclosed. This decision is based on lessons learned during the 2009 novel influenza pandemic whereby it took time to provide care to those who needed urgent attention as many people visited certain medical institutions in some prefectures. This is a necessary response to prioritize the provision of care to those who need urgent attention (i.e. patients with severe symptoms who need intensive care). The government asks for the understanding of the public.
(The reason for the initial negative results of the PCR tests turning positive (in such cases as the cruise ship))
There are several reasons behind the cases that some passengers have tested positive after disembarking from the cruise ship. For instance, it can be considered that, even if a person is infected with the novel coronavirus, the person might test negative as the number of virus particles has not increased enough to exceed the minimum limit of detection at the initial stage of infection. Therefore, when taking the test again after the number of virus particle has sufficiently increased, that person could be tested positive.
PCR screening is now covered by health care insurance so as to facilitate the necessary tests for patients. Those who consult the Call Centers for Japanese Returnees and Potential Contacts (available 24 hours) and for whom it is deemed necessary to conduct screening by the respective outpatient facility for returnees and potential contacts, relayed by the call center, are eligible to request a test directly from one of the private-sector screening institutions without going through a public health center.
When medical doctors find necessary to conduct a PCR test, patients will be referred to outpatient facilities for returnees and potential contacts, and undergo screening based on the determination made by the doctors.
Aiming to prevent the refusal of test requests due to limited local screening capacity, the government will more closely facilitate the process to ensure that each area can conduct the necessary tests by sharing diagnostic reagents among wider areas.
At the same time, new rapid diagnostic test kits have been under development that can significantly shorten testing time.
(Reasons for requesting possible patients refraining from immediately consulting medical institutions)
First and foremost, most of the symptoms of a common cold, fever, lassitude, or difficulty in breathing, at this moment, are being caused by diseases other than the novel coronavirus disease, such as influenza. If a cold or influenza is suspected, it is advised to consult with a family doctor or other doctors nearby as usual.
Meanwhile, suspected patients of novel coronavirus are visiting outpatient facilities for returnees and potential contacts referred by the Call Centers for Japanese Returnees and Potential Contacts; when a person is not actually infected, visiting those medical institutions, which have outpatient facilities, without proper consultation, just because he or she is concerned about having an infection, will increase the risk of infection.
In the event of concern over infection by the novel coronavirus, it is advised to consult with the Call Centers. The list of medical institutions that have the aforementioned outpatient facilities is not disclosed. This decision is based on lessons learned during the 2009 novel influenza pandemic whereby it took time to provide care to those who needed urgent attention as many people visited certain medical institutions in some prefectures. This is a necessary response to prioritize the provision of care to those who need urgent attention (i.e. patients with severe symptoms who need intensive care). The government asks for the understanding of the public.
(The reason for the initial negative results of the PCR tests turning positive (in such cases as the cruise ship))
There are several reasons behind the cases that some passengers have tested positive after disembarking from the cruise ship. For instance, it can be considered that, even if a person is infected with the novel coronavirus, the person might test negative as the number of virus particles has not increased enough to exceed the minimum limit of detection at the initial stage of infection. Therefore, when taking the test again after the number of virus particle has sufficiently increased, that person could be tested positive.